What Can You Do About Fallen Arches?
Overview
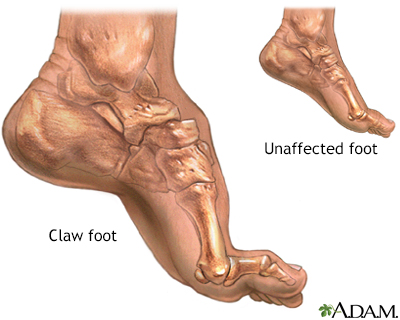
Over-pronation is very common and affects millions of Australians. To better understand this condition, we'll take a closer look at the 3 most common foot types. An estimated 70% of the population has fallen arches (or a low arch). Only 20% has a normal arch. And 10% have abnormal feet, in other words they either have flat feet or the opposite - a high arched foot.
Causes
You can have a tendency towards fallen arches from birth. Up through the toddler stage, it is common to have flat feet. Throughout childhood, arches tend to normally develop. For reasons not well understood, however, in some cases the feet stay flat and the arch never forms. In many cases this abnormality does not cause symptoms or require any treatment. In other cases, it is due to a condition called tarsal coalition. This occurs when some of the foot bones fuse.
Symptoms
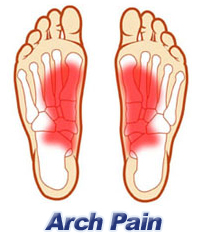
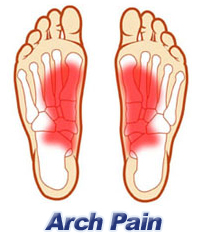
Some people have fallen arches, and they aren?t even aware of it, fallen arches are sometimes asymptomatic and do not always cause pain. However, for others, the following symptoms may be present. Foot pain, particularly in the arches or heels, leg or back pain, feet feel tired quickly, swelling in the feet and difficulty moving the feet.
Diagnosis
If your child has flatfeet, his or her doctor will ask about any family history of flatfeet or inherited foot problems. In a person of any age, the doctor will ask about occupational and recreational activities, previous foot trauma or foot surgery and the type of shoes worn. The doctor will examine your shoes to check for signs of excessive wear. Worn shoes often provide valuable clues to gait problems and poor bone alignment. The doctor will ask you to walk barefoot to evaluate the arches of the feet, to check for out-toeing and to look for other signs of poor foot mechanics. The doctor will examine your feet for foot flexibility and range of motion and feel for any tenderness or bony abnormalities. Depending on the results of this physical examination, foot X-rays may be recommended. X-rays are always performed in a young child with rigid flatfeet and in an adult with acquired flatfeet due to trauma.
bestshoelifts
Non Surgical Treatment
If your condition is bothersome, try elevating your feet and using ice on the arches to reduce swelling. Your podiatrist can recommend several orthotic aids and inserts to strengthen the tendons of your foot. He can also demonstrate stretching exercises or refer you to physical therapy to get those tendons back into shape. If the symptoms of fallen arches are painful and troubling, he may recommend a steroid injection to relieve inflammation and pain. And in some instances, he may determine that surgery is necessary.
Surgical Treatment

This is rare and usually only offered if patients have significant abnormalities in their bones or muscles. Treatments include joint fusion, reshaping the bones in the foot, and occasionally moving around tendons in the foot to help balance out the stresses (called tendon transfer). Flat feet and fallen arches are common conditions that are in most cases asymptomatic. However, in patients who do have symptoms, treatments are available that can help reduce pain and promote efficient movement. Orthotic devices are well recognised as an excellent treatment and podiatrists can offer these different treatment modalities as individualised treatments for patients.
After Care
Time off work depends on the type of work as well as the surgical procedures performed. . A patient will be required to be non-weight bearing in a cast or splint and use crutches for four to twelve weeks. Usually a patient can return to work in one to two weeks if they are able to work while seated. If a person's job requires standing and walking, return to work may take several weeks. Complete recovery may take six months to a full year. Complications can occur as with all surgeries, but are minimized by strictly following your surgeon's post-operative instructions. The main complications include infection, bone that is slow to heal or does not heal, progression or reoccurrence of deformity, a stiff foot, and the need for further surgery. Many of the above complications can be avoided by only putting weight on the operative foot when allowed by your surgeon.
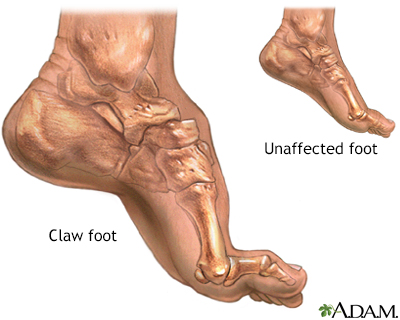
Over-pronation is very common and affects millions of Australians. To better understand this condition, we'll take a closer look at the 3 most common foot types. An estimated 70% of the population has fallen arches (or a low arch). Only 20% has a normal arch. And 10% have abnormal feet, in other words they either have flat feet or the opposite - a high arched foot.
Causes
You can have a tendency towards fallen arches from birth. Up through the toddler stage, it is common to have flat feet. Throughout childhood, arches tend to normally develop. For reasons not well understood, however, in some cases the feet stay flat and the arch never forms. In many cases this abnormality does not cause symptoms or require any treatment. In other cases, it is due to a condition called tarsal coalition. This occurs when some of the foot bones fuse.
Symptoms
Some people have fallen arches, and they aren?t even aware of it, fallen arches are sometimes asymptomatic and do not always cause pain. However, for others, the following symptoms may be present. Foot pain, particularly in the arches or heels, leg or back pain, feet feel tired quickly, swelling in the feet and difficulty moving the feet.
Diagnosis
If your child has flatfeet, his or her doctor will ask about any family history of flatfeet or inherited foot problems. In a person of any age, the doctor will ask about occupational and recreational activities, previous foot trauma or foot surgery and the type of shoes worn. The doctor will examine your shoes to check for signs of excessive wear. Worn shoes often provide valuable clues to gait problems and poor bone alignment. The doctor will ask you to walk barefoot to evaluate the arches of the feet, to check for out-toeing and to look for other signs of poor foot mechanics. The doctor will examine your feet for foot flexibility and range of motion and feel for any tenderness or bony abnormalities. Depending on the results of this physical examination, foot X-rays may be recommended. X-rays are always performed in a young child with rigid flatfeet and in an adult with acquired flatfeet due to trauma.
bestshoelifts
Non Surgical Treatment
If your condition is bothersome, try elevating your feet and using ice on the arches to reduce swelling. Your podiatrist can recommend several orthotic aids and inserts to strengthen the tendons of your foot. He can also demonstrate stretching exercises or refer you to physical therapy to get those tendons back into shape. If the symptoms of fallen arches are painful and troubling, he may recommend a steroid injection to relieve inflammation and pain. And in some instances, he may determine that surgery is necessary.
Surgical Treatment

This is rare and usually only offered if patients have significant abnormalities in their bones or muscles. Treatments include joint fusion, reshaping the bones in the foot, and occasionally moving around tendons in the foot to help balance out the stresses (called tendon transfer). Flat feet and fallen arches are common conditions that are in most cases asymptomatic. However, in patients who do have symptoms, treatments are available that can help reduce pain and promote efficient movement. Orthotic devices are well recognised as an excellent treatment and podiatrists can offer these different treatment modalities as individualised treatments for patients.
After Care
Time off work depends on the type of work as well as the surgical procedures performed. . A patient will be required to be non-weight bearing in a cast or splint and use crutches for four to twelve weeks. Usually a patient can return to work in one to two weeks if they are able to work while seated. If a person's job requires standing and walking, return to work may take several weeks. Complete recovery may take six months to a full year. Complications can occur as with all surgeries, but are minimized by strictly following your surgeon's post-operative instructions. The main complications include infection, bone that is slow to heal or does not heal, progression or reoccurrence of deformity, a stiff foot, and the need for further surgery. Many of the above complications can be avoided by only putting weight on the operative foot when allowed by your surgeon.
Leg Length Discrepancy Tests
Overview
The two major categorizations of LLD are structural and functional. A third more minor category is environmental. In structural LLD there is an actual anatomical difference in the bones of the lower extremities where one side becomes shorter than the other. This type of LLD may be genetic, where the person is born in this way. In other cases it may be due to injury or infection through the growth phases of early childhood or adolescence. Some spinal abnormalities like scoliosis can also cause this condition. Functional LLD is where the bones are not the cause of difference but a muscle or pelvic condition has the effect of weakening the leg on one side. Conditions that can cause this are muscle inflexibility, adduction contractures and pelvic obliquity (amongst others). The third less severe category of environmental LLD is caused by discrepancies in the surface that the feet and legs are resting or walking on. Banked, uneven or curved surfaces can all cause environmental LLD. In LLD the asymmetric nature of the legs in relation to hips and back caused the centre of gravity to shift from its natural position. This then results in the body attempting to compensate by either tilting the pelvic areas towards the shorter side, increased knee flexing on the longer side, flexion of the ankle plantar and foot supination towards the shorter side.
Causes
Leg length discrepancies can be caused by poor alignment of the pelvis or simply because one leg is structurally longer than the other. Regardless of the reason, your body wants to be symmetrical and will do its best to compensate for the length difference. The greater the leg length difference, the earlier the symptoms will present themselves to the patient. Specific diagnoses that coincide with leg length discrepancy include: scoliosis, lumbar herniated discs, sacroiliitis, pelvic obiliquity, greater trochanteric bursitis, hip arthritis, piriformis syndrome, patellofemoral syndrome and foot pronation. Other potential causes could be due to an injury (such as a fracture), bone disease, bone tumors, congenital problems (present at birth) or from a neuromuscular problem.
Symptoms
Faulty feet and ankle structure profoundly affect leg length and pelvic positioning. The most common asymmetrical foot position is the pronated foot. Sensory receptors embedded on the bottom of the foot alert the brain to the slightest weight shift. Since the brain is always trying to maintain pelvic balance, when presented with a long left leg, it attempts to adapt to the altered weight shift by dropping the left medial arch (shortening the long leg) and supinating the right arch to lengthen the short leg.1 Left unchecked, excessive foot pronation will internally rotate the left lower extremity, causing excessive strain to the lateral meniscus and medial collateral knee ligaments. Conversely, excessive supination tends to externally rotate the leg and thigh, creating opposite knee, hip and pelvic distortions.
Diagnosis
A doctor will generally take a detailed medical history of both the patient and family, including asking about recent injuries or illnesses. He or she will carefully examine the patient, observing how he or she moves and stands. If necessary, an orthopedic surgeon will order X-ray, bone age determinations and computed tomography (CT) scans or magnetic resonance imaging (MRI).
Non Surgical Treatment
In some circumstances, the physician will recommend a non-surgical form of treatment. Non-surgical treatments include orthotics and prosthetics. Orthotics are a special type of lift placed in or on a shoe that can be used in the treatment of leg length discrepancies between two and six centimeters. In pediatric patients who have large discrepancies and are not good candidates for other treatment forms, prosthetics can be helpful.

shoe lifts for men's shoes
Surgical Treatment
Surgical options in leg length discrepancy treatment include procedures to lengthen the shorter leg, or shorten the longer leg. Your child's physician will choose the safest and most effective method based on the aforementioned factors. No matter the surgical procedure performed, physical therapy will be required after surgery in order to stretch muscles and help support the flexibility of the surrounding joints. Surgical shortening is safer than surgical lengthening and has fewer complications. Surgical procedures to shorten one leg include removing part of a bone, called a bone resection. They can also include epiphysiodesis or epiphyseal stapling, where the growth plate in a bone is tethered or stapled. This slows the rate of growth in the surgical leg.
The two major categorizations of LLD are structural and functional. A third more minor category is environmental. In structural LLD there is an actual anatomical difference in the bones of the lower extremities where one side becomes shorter than the other. This type of LLD may be genetic, where the person is born in this way. In other cases it may be due to injury or infection through the growth phases of early childhood or adolescence. Some spinal abnormalities like scoliosis can also cause this condition. Functional LLD is where the bones are not the cause of difference but a muscle or pelvic condition has the effect of weakening the leg on one side. Conditions that can cause this are muscle inflexibility, adduction contractures and pelvic obliquity (amongst others). The third less severe category of environmental LLD is caused by discrepancies in the surface that the feet and legs are resting or walking on. Banked, uneven or curved surfaces can all cause environmental LLD. In LLD the asymmetric nature of the legs in relation to hips and back caused the centre of gravity to shift from its natural position. This then results in the body attempting to compensate by either tilting the pelvic areas towards the shorter side, increased knee flexing on the longer side, flexion of the ankle plantar and foot supination towards the shorter side.

Causes
Leg length discrepancies can be caused by poor alignment of the pelvis or simply because one leg is structurally longer than the other. Regardless of the reason, your body wants to be symmetrical and will do its best to compensate for the length difference. The greater the leg length difference, the earlier the symptoms will present themselves to the patient. Specific diagnoses that coincide with leg length discrepancy include: scoliosis, lumbar herniated discs, sacroiliitis, pelvic obiliquity, greater trochanteric bursitis, hip arthritis, piriformis syndrome, patellofemoral syndrome and foot pronation. Other potential causes could be due to an injury (such as a fracture), bone disease, bone tumors, congenital problems (present at birth) or from a neuromuscular problem.
Symptoms
Faulty feet and ankle structure profoundly affect leg length and pelvic positioning. The most common asymmetrical foot position is the pronated foot. Sensory receptors embedded on the bottom of the foot alert the brain to the slightest weight shift. Since the brain is always trying to maintain pelvic balance, when presented with a long left leg, it attempts to adapt to the altered weight shift by dropping the left medial arch (shortening the long leg) and supinating the right arch to lengthen the short leg.1 Left unchecked, excessive foot pronation will internally rotate the left lower extremity, causing excessive strain to the lateral meniscus and medial collateral knee ligaments. Conversely, excessive supination tends to externally rotate the leg and thigh, creating opposite knee, hip and pelvic distortions.
Diagnosis
A doctor will generally take a detailed medical history of both the patient and family, including asking about recent injuries or illnesses. He or she will carefully examine the patient, observing how he or she moves and stands. If necessary, an orthopedic surgeon will order X-ray, bone age determinations and computed tomography (CT) scans or magnetic resonance imaging (MRI).
Non Surgical Treatment
In some circumstances, the physician will recommend a non-surgical form of treatment. Non-surgical treatments include orthotics and prosthetics. Orthotics are a special type of lift placed in or on a shoe that can be used in the treatment of leg length discrepancies between two and six centimeters. In pediatric patients who have large discrepancies and are not good candidates for other treatment forms, prosthetics can be helpful.

shoe lifts for men's shoes
Surgical Treatment
Surgical options in leg length discrepancy treatment include procedures to lengthen the shorter leg, or shorten the longer leg. Your child's physician will choose the safest and most effective method based on the aforementioned factors. No matter the surgical procedure performed, physical therapy will be required after surgery in order to stretch muscles and help support the flexibility of the surrounding joints. Surgical shortening is safer than surgical lengthening and has fewer complications. Surgical procedures to shorten one leg include removing part of a bone, called a bone resection. They can also include epiphysiodesis or epiphyseal stapling, where the growth plate in a bone is tethered or stapled. This slows the rate of growth in the surgical leg.
What Are The Major Causes Of Heel Soreness
Overview

The heel is a cushion of fatty tissue that protects the structures of the foot, including the heel bone, muscles and ligaments. Heel pain is a common foot complaint. Complications include plantar fasciitis and heel spurs. Sever's disease is a common cause of heel pain in children. A podiatrist can help diagnose and treat heel pain. The heel is a padded cushion of fatty tissue around the heel bone (the calcaneus) that holds its shape despite the pressure of body weight and movement. It serves to protect the structures of the foot, including the calcaneus, muscles and ligaments. Heel pain is a very common foot complaint. Anyone can suffer from heel pain, but certain groups seem to be at increased risk, including, middle-aged men and women, physically active people, people who are overweight or obese, people who are on their feet for long periods of time, children aged between eight and 13 years (particularly boys) and women during pregnancy.
Causes
Common causes of heel pain include Achilles tendinitis, Achilles tendon rupture, Bone tumor, Bursitis, Fibromyalgia, Fracture, Gout, Heel pad wear and tear, Heel spur, Osteomyelitis, Peripheral neuropathy, Pinched nerve, Plantar fasciitis, Rheumatoid arthritis, Stress fractures, Tarsal tunnel syndrome, Tendinitis. Causes shown here are commonly associated with this symptom. Work with your doctor or other health care professional for an accurate diagnosis.
Symptoms
Usually worse with the first few steps in the morning or at the initial point of activity. The latter usually gets better with continued activity (squeaky hinge analogy). Walking, running, sprinting, hill running and jumping will increase the pain. Often, the natural response is to walk on the outside of the foot - in supination - to lessen the stress on the plantar fascia - resulting in new problems.
Diagnosis
A biomechanical exam by your podiatrist will help reveal these abnormalities and in turn resolve the cause of plantar fasciitis. By addressing this cause, the patient can be offered a podiatric long-term solution to his problem.
Non Surgical Treatment
There are many treatments for fasciitis. The most common initial treatment provided by the family doctor are anti-inflammatory medications. They may take the edge off the pain, but they don't often resolve the condition fully. Steroid injections, which deliver the medication directly to the most painful area, are usually more effective. Rest, ice, weight loss, taping, strapping, immobilization, physiotherapy, massage, stretching, heel cushions, acupuncture, night splints and extra-corporeal shock wave therapy all help some patients. Many patients, however, have a biomechanical cause such as excessively pronated feet to their complaint, and this may mean many of the treatments listed above will only provide temporary relief of fasciitis symptoms. When you stop the treatment, the pain often returns. This is why many cases of fasciitis respond well to orthoses, custom-made inserts that control the mechanical cause of the complaint. If you're considering orthoses, it's very important to have a podiatrist specializing in the field to examine you. There are many biomechanical factors to consider when assessing the need for literally dozens of types of devices available, so you need to have an expert to properly assess you. (Unfortunately, as is the case in many jurisdictions, there is no minimum standard of training required in British Columbia to make orthoses, and there are many fly-by-night operations around that employ salesmen with little, if any, training in understanding anatomy or foot function. The emphasis with these groups is on selling you some sort of device, rather than providing proper assessment, treatment and follow-up.
Surgical Treatment
With the advancements in technology and treatments, if you do need to have surgery for the heel, it is very minimal incision that?s done. And the nice thing is your recovery period is short and you should be able to bear weight right after the surgery. This means you can get back to your weekly routine in just a few weeks. Recovery is a lot different than it used to be and a lot of it is because of doing a minimal incision and decreasing trauma to soft tissues, as well as even the bone. So if you need surgery, then your recovery period is pretty quick.
heelsncleavage
Prevention
Wear shoes that fit well, front, back and sides and have shock-absorbent soles, rigid uppers and supportive heel counters. Do not wear shoes with excessive wear on heels or soles. Prepare properly before exercising. Warm-up before running or walking, and do some stretching exercises afterward. Pace yourself when you participate in athletic activities. If overweight, try non weight-bearing activities such as swimming or cycling. Your podiatrist may also use taping or strapping to provide extra support for your foot. Orthoses (shoe inserts) specifically made to suit your needs may be also be prescribed.

The heel is a cushion of fatty tissue that protects the structures of the foot, including the heel bone, muscles and ligaments. Heel pain is a common foot complaint. Complications include plantar fasciitis and heel spurs. Sever's disease is a common cause of heel pain in children. A podiatrist can help diagnose and treat heel pain. The heel is a padded cushion of fatty tissue around the heel bone (the calcaneus) that holds its shape despite the pressure of body weight and movement. It serves to protect the structures of the foot, including the calcaneus, muscles and ligaments. Heel pain is a very common foot complaint. Anyone can suffer from heel pain, but certain groups seem to be at increased risk, including, middle-aged men and women, physically active people, people who are overweight or obese, people who are on their feet for long periods of time, children aged between eight and 13 years (particularly boys) and women during pregnancy.
Causes
Common causes of heel pain include Achilles tendinitis, Achilles tendon rupture, Bone tumor, Bursitis, Fibromyalgia, Fracture, Gout, Heel pad wear and tear, Heel spur, Osteomyelitis, Peripheral neuropathy, Pinched nerve, Plantar fasciitis, Rheumatoid arthritis, Stress fractures, Tarsal tunnel syndrome, Tendinitis. Causes shown here are commonly associated with this symptom. Work with your doctor or other health care professional for an accurate diagnosis.
Symptoms
Usually worse with the first few steps in the morning or at the initial point of activity. The latter usually gets better with continued activity (squeaky hinge analogy). Walking, running, sprinting, hill running and jumping will increase the pain. Often, the natural response is to walk on the outside of the foot - in supination - to lessen the stress on the plantar fascia - resulting in new problems.
Diagnosis
A biomechanical exam by your podiatrist will help reveal these abnormalities and in turn resolve the cause of plantar fasciitis. By addressing this cause, the patient can be offered a podiatric long-term solution to his problem.
Non Surgical Treatment
There are many treatments for fasciitis. The most common initial treatment provided by the family doctor are anti-inflammatory medications. They may take the edge off the pain, but they don't often resolve the condition fully. Steroid injections, which deliver the medication directly to the most painful area, are usually more effective. Rest, ice, weight loss, taping, strapping, immobilization, physiotherapy, massage, stretching, heel cushions, acupuncture, night splints and extra-corporeal shock wave therapy all help some patients. Many patients, however, have a biomechanical cause such as excessively pronated feet to their complaint, and this may mean many of the treatments listed above will only provide temporary relief of fasciitis symptoms. When you stop the treatment, the pain often returns. This is why many cases of fasciitis respond well to orthoses, custom-made inserts that control the mechanical cause of the complaint. If you're considering orthoses, it's very important to have a podiatrist specializing in the field to examine you. There are many biomechanical factors to consider when assessing the need for literally dozens of types of devices available, so you need to have an expert to properly assess you. (Unfortunately, as is the case in many jurisdictions, there is no minimum standard of training required in British Columbia to make orthoses, and there are many fly-by-night operations around that employ salesmen with little, if any, training in understanding anatomy or foot function. The emphasis with these groups is on selling you some sort of device, rather than providing proper assessment, treatment and follow-up.
Surgical Treatment
With the advancements in technology and treatments, if you do need to have surgery for the heel, it is very minimal incision that?s done. And the nice thing is your recovery period is short and you should be able to bear weight right after the surgery. This means you can get back to your weekly routine in just a few weeks. Recovery is a lot different than it used to be and a lot of it is because of doing a minimal incision and decreasing trauma to soft tissues, as well as even the bone. So if you need surgery, then your recovery period is pretty quick.
heelsncleavage
Prevention
Wear shoes that fit well, front, back and sides and have shock-absorbent soles, rigid uppers and supportive heel counters. Do not wear shoes with excessive wear on heels or soles. Prepare properly before exercising. Warm-up before running or walking, and do some stretching exercises afterward. Pace yourself when you participate in athletic activities. If overweight, try non weight-bearing activities such as swimming or cycling. Your podiatrist may also use taping or strapping to provide extra support for your foot. Orthoses (shoe inserts) specifically made to suit your needs may be also be prescribed.
Coping with Mortons Neuroma
Overview
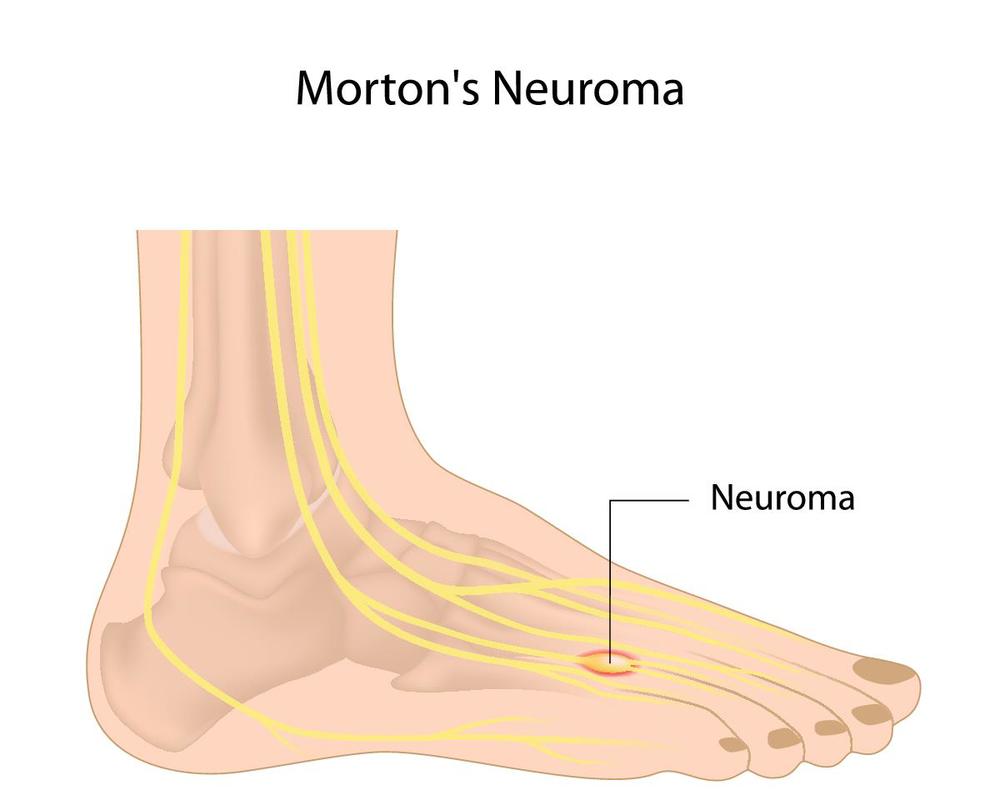 During certain activities, particularly weight-bearing activities (e.g. walking or running) a compressive force, is sometimes placed on the interdigital nerves and surrounding soft tissue, between the metatarsal bones (this is often the case with tight fitting shoes or in patients with flat feet). If this force is repetitive enough and beyond what the nerve and soft tissue can withstand, swelling to the nerve and soft tissue may occur. This may result in pain, tenderness, pins and needles or numbness in the forefoot or toes. When this happens, the condition is known as a Morton's neuroma.
During certain activities, particularly weight-bearing activities (e.g. walking or running) a compressive force, is sometimes placed on the interdigital nerves and surrounding soft tissue, between the metatarsal bones (this is often the case with tight fitting shoes or in patients with flat feet). If this force is repetitive enough and beyond what the nerve and soft tissue can withstand, swelling to the nerve and soft tissue may occur. This may result in pain, tenderness, pins and needles or numbness in the forefoot or toes. When this happens, the condition is known as a Morton's neuroma.
Causes
Anything that causes compression or irritation of the nerve can lead to the development of a neuroma. One of the most common causes comes from wearing shoes that have a tapered toe box, or high-heeled shoes that cause the toes to be forced into the toe box and overload pressure onto the forefoot. An injury or trauma to the forefoot may also lead to a neuroma. People at a higher risk of developing a Neuroma include people with certain foot deformities, such as bunions or hammertoes. Certain foot types, such as flat feet (Pronation) More flexible feet, and woman after pregnancy.
Symptoms
Patients with a Morton's neuroma typically experience a sharp, shooting or burning pain, usually at the base of the forefoot or toes, which radiates into the two affected toes. Sometimes the pain may also radiate into the foot. The pain is often associated with the presence of pins and needles and numbness.
Diagnosis
Based on the physical examination, your doctor usually can diagnose a Morton's neuroma without additional testing. A foot X-ray may be ordered to make sure that there isn't a stress fracture, but it will not show the actual neuroma. If the diagnosis is in doubt, your doctor may request magnetic resonance imaging (MRI) of the foot.
Non Surgical Treatment
Initial treatment for Morton?s Neuroma may include non-prescription anti-inflammatory medications to reduce pain and swelling. These may consist of standard analgesics such as aspirin and ibuprofen (Advil, Motrin, others). Massaging the painful region three times daily with ice. Change of footwear. Avoid tight shoes, high heels or any footwear that seems to irritate the condition. Low heeled shoes with softer soles are preferable. Arch supports and foot pads to help reduce pressure on the nerve. In some cases, a physician may prescribe a customized shoe insert, molded to fit the contours of the patient?s foot. Reducing activities causing stress to the foot, including jogging, dancing, aerobic activity or any high impact movements of the foot. Injections of a corticosteroid medication to reduce the swelling and inflammation of the nerve and reduce pain. Occasionally other substances may be injected in order to ?ablate? the Neuroma. (The overuse of injected steroids is to be avoided however, as side effects, including weight gain and high blood pressure can result.)
Surgical Treatment
Operative treatment of Morton?s neuroma should be entertained only after failure of nonoperative management. Standard operative treatment involves identifying the nerve and cutting (resecting) it proximal to the point where it is irritate/injured. This is usually done through an incision on the top (dorsal) aspect of the foot, although in rare instances, an incision on the sole (plantar) aspect of the foot maybe used. An incision on the sole of the foot works very well, unless an excessive scar forms in which case it can be problematic. Some physicians will attempt to treat Morton?s neuroma by releasing the intermetatarsal ligament and freeing the nerve of local scar tissue. This may also be beneficial.
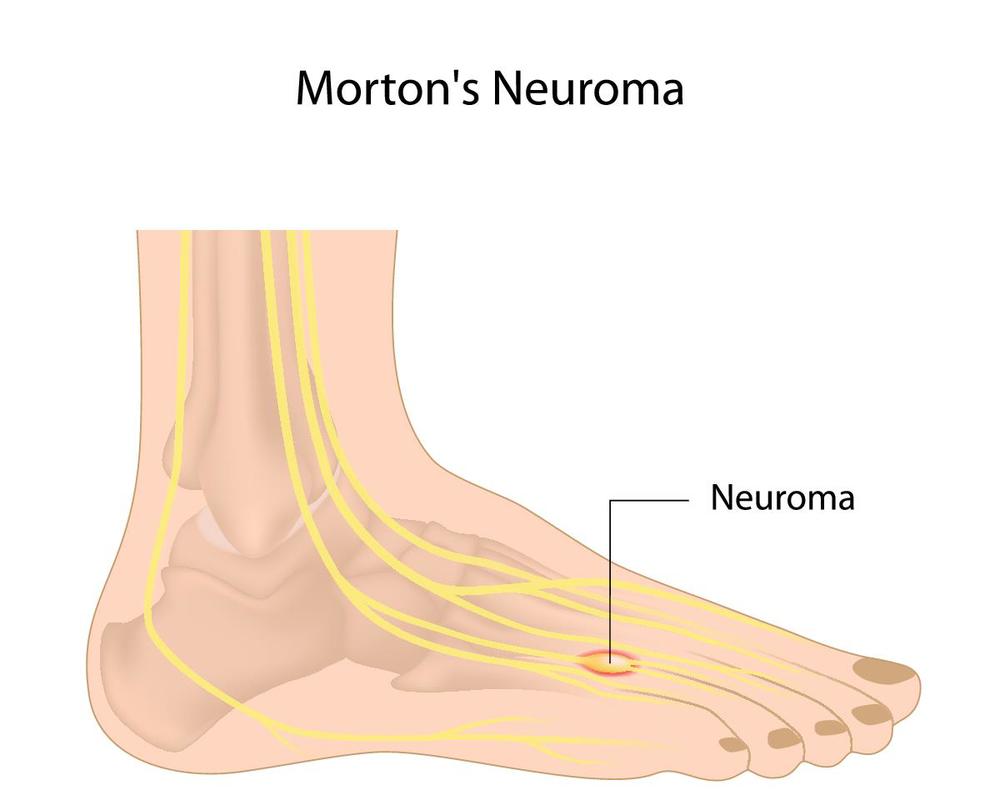 During certain activities, particularly weight-bearing activities (e.g. walking or running) a compressive force, is sometimes placed on the interdigital nerves and surrounding soft tissue, between the metatarsal bones (this is often the case with tight fitting shoes or in patients with flat feet). If this force is repetitive enough and beyond what the nerve and soft tissue can withstand, swelling to the nerve and soft tissue may occur. This may result in pain, tenderness, pins and needles or numbness in the forefoot or toes. When this happens, the condition is known as a Morton's neuroma.
During certain activities, particularly weight-bearing activities (e.g. walking or running) a compressive force, is sometimes placed on the interdigital nerves and surrounding soft tissue, between the metatarsal bones (this is often the case with tight fitting shoes or in patients with flat feet). If this force is repetitive enough and beyond what the nerve and soft tissue can withstand, swelling to the nerve and soft tissue may occur. This may result in pain, tenderness, pins and needles or numbness in the forefoot or toes. When this happens, the condition is known as a Morton's neuroma.Causes
Anything that causes compression or irritation of the nerve can lead to the development of a neuroma. One of the most common causes comes from wearing shoes that have a tapered toe box, or high-heeled shoes that cause the toes to be forced into the toe box and overload pressure onto the forefoot. An injury or trauma to the forefoot may also lead to a neuroma. People at a higher risk of developing a Neuroma include people with certain foot deformities, such as bunions or hammertoes. Certain foot types, such as flat feet (Pronation) More flexible feet, and woman after pregnancy.
Symptoms
Patients with a Morton's neuroma typically experience a sharp, shooting or burning pain, usually at the base of the forefoot or toes, which radiates into the two affected toes. Sometimes the pain may also radiate into the foot. The pain is often associated with the presence of pins and needles and numbness.
Diagnosis
Based on the physical examination, your doctor usually can diagnose a Morton's neuroma without additional testing. A foot X-ray may be ordered to make sure that there isn't a stress fracture, but it will not show the actual neuroma. If the diagnosis is in doubt, your doctor may request magnetic resonance imaging (MRI) of the foot.
Non Surgical Treatment
Initial treatment for Morton?s Neuroma may include non-prescription anti-inflammatory medications to reduce pain and swelling. These may consist of standard analgesics such as aspirin and ibuprofen (Advil, Motrin, others). Massaging the painful region three times daily with ice. Change of footwear. Avoid tight shoes, high heels or any footwear that seems to irritate the condition. Low heeled shoes with softer soles are preferable. Arch supports and foot pads to help reduce pressure on the nerve. In some cases, a physician may prescribe a customized shoe insert, molded to fit the contours of the patient?s foot. Reducing activities causing stress to the foot, including jogging, dancing, aerobic activity or any high impact movements of the foot. Injections of a corticosteroid medication to reduce the swelling and inflammation of the nerve and reduce pain. Occasionally other substances may be injected in order to ?ablate? the Neuroma. (The overuse of injected steroids is to be avoided however, as side effects, including weight gain and high blood pressure can result.)

Surgical Treatment
Operative treatment of Morton?s neuroma should be entertained only after failure of nonoperative management. Standard operative treatment involves identifying the nerve and cutting (resecting) it proximal to the point where it is irritate/injured. This is usually done through an incision on the top (dorsal) aspect of the foot, although in rare instances, an incision on the sole (plantar) aspect of the foot maybe used. An incision on the sole of the foot works very well, unless an excessive scar forms in which case it can be problematic. Some physicians will attempt to treat Morton?s neuroma by releasing the intermetatarsal ligament and freeing the nerve of local scar tissue. This may also be beneficial.
Shoe Lifts The Chiropodists Treatment For Leg Length Discrepancy
There are actually two unique variations of leg length discrepancies, congenital and acquired. Congenital indicates you are born with it. One leg is anatomically shorter compared to the other. As a result of developmental stages of aging, the brain senses the stride pattern and identifies some variation. The entire body typically adapts by tilting one shoulder to the "short" side. A difference of under a quarter inch is not very uncommon, doesn't need Shoe Lifts to compensate and usually won't have a serious effect over a lifetime.

Leg length inequality goes largely undiagnosed on a daily basis, however this issue is simply corrected, and can reduce quite a few instances of upper back pain.
Treatment for leg length inequality commonly consists of Shoe Lifts . They are cost-effective, ordinarily priced at less than twenty dollars, compared to a custom orthotic of $200 or even more. When the amount of leg length inequality begins to exceed half an inch, a whole sole lift is generally the better choice than a heel lift. This prevents the foot from being unnecessarily stressed in an abnormal position.
Back pain is easily the most common ailment afflicting men and women today. Over 80 million people are affected by back pain at some point in their life. It is a problem that costs employers vast amounts of money each year because of lost time and output. Innovative and more effective treatment methods are constantly sought after in the hope of minimizing the economic impact this issue causes.

People from all corners of the earth suffer the pain of foot ache as a result of leg length discrepancy. In these types of cases Shoe Lifts can be of worthwhile. The lifts are capable of easing any pain in the feet. Shoe Lifts are recommended by many expert orthopaedic practitioners".
In order to support the body in a well balanced manner, your feet have a very important part to play. Despite that, it's often the most overlooked area in the body. Many people have flat-feet which means there may be unequal force exerted on the feet. This will cause other parts of the body including knees, ankles and backs to be impacted too. Shoe Lifts ensure that ideal posture and balance are restored.

Leg length inequality goes largely undiagnosed on a daily basis, however this issue is simply corrected, and can reduce quite a few instances of upper back pain.
Treatment for leg length inequality commonly consists of Shoe Lifts . They are cost-effective, ordinarily priced at less than twenty dollars, compared to a custom orthotic of $200 or even more. When the amount of leg length inequality begins to exceed half an inch, a whole sole lift is generally the better choice than a heel lift. This prevents the foot from being unnecessarily stressed in an abnormal position.
Back pain is easily the most common ailment afflicting men and women today. Over 80 million people are affected by back pain at some point in their life. It is a problem that costs employers vast amounts of money each year because of lost time and output. Innovative and more effective treatment methods are constantly sought after in the hope of minimizing the economic impact this issue causes.

People from all corners of the earth suffer the pain of foot ache as a result of leg length discrepancy. In these types of cases Shoe Lifts can be of worthwhile. The lifts are capable of easing any pain in the feet. Shoe Lifts are recommended by many expert orthopaedic practitioners".
In order to support the body in a well balanced manner, your feet have a very important part to play. Despite that, it's often the most overlooked area in the body. Many people have flat-feet which means there may be unequal force exerted on the feet. This will cause other parts of the body including knees, ankles and backs to be impacted too. Shoe Lifts ensure that ideal posture and balance are restored.
Will A Calcaneal Spur Cause Pain?

Overview
Heel spurs occur in at least half the people who have plantar fasciitis, a painful condition involving the thick tissue that runs between your heel bone and your toes. In the past, doctors often performed surgery to remove heel spurs, believing them to be the cause of the pain associated with plantar fasciitis. In treating plantar fasciitis now, doctors rely more on ice, arch supports, physical therapy and pain medications, and surgery is rarely performed.
Causes
When the Plantar Fascia is allowed to rest during sleep or long periods of inactivity, the fascia tightens and shortens. When you first stand up after resting, the fascia is forced to stretch very quickly causing micro-tears in the tissue. This is why the first steps in the morning are so exquisitely painful. Heel spurs are more likely to happen if you suffer from over-pronation (walking with a rolling gait) you stand or walk on rigid surfaces for long periods, you are above ideal weight or during pregnancy, you have stiff muscles in your calves.

Symptoms
Symptoms may be similar to those of plantar fasciitis and include pain and tenderness at the base of the heel, pain on weight bearing and in severe cases difficulty walking. The main diagnosis of a heel spur is made by X-ray where a bony growth on the heel can be seen. A heel spur can occur without any symptoms at all and the athlete would never know they have the bony growth on the heel. Likewise, Plantar fasciitis can occur without the bone growth present.
Diagnosis
A heel spur is often seen on X-ray as a bony protrusion, which can vary in size. However, because a Heel Spur only indicates increased load on the plantar fascia, and not pain, an ultra sound may be required to assess other actual cause of the heel pain such and may include checking to see if the plantar fascia is inflamed or degenerated.
Non Surgical Treatment
Elevation of the affected foot and leg at rest may diminish the pain. Applying gentle heat to the painful area may ease the pain by dilating local blood vessels. One also can protect the heel by placing a foam rubber pad in the heel of the shoe. A pad about one-half inch thick will raise the heel, shift the weight of the body forward, and protect the irritated muscles attached to the heel bone. The same effect can be achieved by using adhesive tape to turn the foot inward. Additional treatment may consist of a number of physical therapies, such as diathermy, ultrasound waves and whirlpool baths.
Surgical Treatment
Usually, heel spurs are curable with conservative treatment. If not, heel spurs are curable with surgery, although there is the possibility of them growing back. About 10% of those who continue to see a physician for plantar fascitis have it for more than a year. If there is limited success after approximately one year of conservative treatment, patients are often advised to have surgery.
Does A Heel Spur Cause Pain?

Overview
In the setting of plantar fasciitis, heel spurs are most often seen in middle-aged men and women, but can be found in all age groups. The heel spur itself is not thought to be the primary cause of pain, rather inflammation and irritation of the plantar fascia is thought to be the primary problem. A heel spur diagnosis is made when an x-ray shows a hook of bone protruding from the bottom of the foot at the point where the plantar fascia is attached to the heel bone.
Causes
Bone spurs form in the feet in response to tight ligaments, to activities such as dancing and running that put stress on the feet, and to pressure from being overweight or from poorly fitting shoes. For example, the long ligament on the bottom of the foot (plantar fascia) can become stressed or tight and pull on the heel, causing the ligament to become inflamed (plantar fasciitis). As the bone tries to mend itself, a bone spur can form on the bottom of the heel (known as a ?heel spur?). Pressure at the back of the heel from frequently wearing shoes that are too tight can cause a bone spur on the back of the heel. This is sometimes called a ?pump bump,? because it is often seen in women who wear high heels.

Symptoms
Heel spurs often do not show any symptoms. If you have intermittent or chronic pain when you walk, run or jog, it may be heel spur. There will be inflammation the point where spur formation happens. The pain is caused by soft tissue injury in the heel. Patients often describe the pain as a pin or knife sticking to the heel. The pain is more specially in the morning when the patient stands up for the first time.
Diagnosis
Most patients who are suffering with heel spurs can see them with an X-ray scan. They are normally hooked and extend into the heel. Some people who have heel spur may not even have noticeable symptoms, although could still be able to see a spur in an X-ray scan.
Non Surgical Treatment
Initially, treatment usually consists of a combination of ice therapy, stretching exercises to improve flexibility (especially in the mornings), anti-inflammatory medications, and physical therapy. Most patients will also need custom-molded orthotics to help control the motion in the foot and arch, which takes the strain off the plantar fascia. If the pain continues, a cortisone injection may be used to calm the severe swelling and pain. There may the need for a night splint to maintain a stretch in the plantar fascia throughout the night.
Surgical Treatment
Most studies indicate that 95% of those afflicted with heel spurs are able to relieve their heel pain with nonsurgical treatments. If you are one of the few people whose symptoms don?t improve with other treatments, your doctor may recommend plantar fascia release surgery. Plantar fascia release involves cutting part of the plantar fascia ligament in order to release the tension and relieve the inflammation of the ligament. Sometimes the bone spur is also removed, if there is a large spur (remember that the bone spur is rarely a cause of pain. Overall, the success rate of surgical release is 70 to 90 percent in patients with heel spurs. One should always be sure to understand all the risks associated with any surgery they are considering.
Prevention
Use orthotic inserts. You can purchase orthotics over the counter, or you can have orthotics specially fitted by your podiatrist. Try 1 of these options. Heel cups. These inserts will help to align the bones in your foot and to cushion your heel. Check your skin for blisters when you first start using heel cups. Also, your feet may sweat more with a heel cup, so change your socks and shoes often. Insoles. While you can pick up generic insoles at a drugstore, you may have more luck if you go to a store that sells athletic shoes. Push on the arch to make sure that it doesn't collapse. If your insoles help but could use a little work, you can take them to a podiatrist to get them customized. Custom orthotics. A podiatrist can make a cast of your foot and provide you with custom-made orthotics. These may be more expensive, but they are made of materials specifically designed for your needs, and they can last up to 5 years if your podiatrist refurbishes them every 1 or 2 years. To find a podiatrist near you, look at the Web page for the American Academy of Podiatric Sports Medicine. Dynamic Insoles. Lack of elasticity in plantar fascia in the foot is for most people the real problem. If there is poor elasticity in the lengthwise tendons in the foot (plantar fascia) in relation to a person's general condition, only a small additional strain is required for the pull on the tendons to cause damage to the tissues connecting the tendons to the heel bone. This will generate an inflamed condition called Plantar Fasciitis.